In the pop culture of the ’60s, tie-dye attired hippies gathered in San Francisco’s Haight-Asbury district to smoke pot, protest the war in Viet Nam and advocate for civil rights. And though activism continued, attire evolved to faded denims, the preppy J. Crew look and Mad Men suits. Over the next two decades or so, cannabis, though still illegal, became socially acceptable replacing the martini at cocktail parties.
In 1996, California passed Proposition 215—the Compassionate Use Act—legalizing cannabis for medical purposes. For the next 32 years not much happened legally. Then, on January 1, 2018, California legalized cannabis for recreational use with Proposition 64. Demand skyrocketed—though not in the way most expected. Aging Baby Boomers, seeking natural, non-toxic, non-addictive medicinal cannabis relief for a range of ailments, drove the market. Passionate users claimed that cannabis worked better than over-the-counter or prescription medications—and without the side effects. So is all the excitement just more “fake news”—or is it for real?
The history of cannabis
For more than 5,000 years, cannabis has been used in many cultures for medicinal purposes. The history of cannabis in the U.S., however, has been fraught with politics and misconceptions. Prior to 1937, cannabis was available in the U.S. for both medicinal and recreational use. Then Congress passed the Marijuana Tax Act prohibiting the sale and use of cannabis, or marijuana, for any purpose. Though the act was subsequently deemed unconstitutional, it was replaced by the Controlled Substances Act with Schedules that ranked substances according to their potential for addiction. Cannabis was placed on Schedule 1, alongside heroin.
Recently, and despite the Federal government’s ongoing prohibition, 33 states and the District of Columbia have passed legislation approving cannabis for medicinal use. It’s expected that more states will soon follow. The U.S. Food and Drug Administration is moving ahead too, albeit slowly. In June 2018, the FDA approved Epidiolex, a cannabidiol oral solution for the treatment of seizures related to two severe rare forms of epilepsy, Lennox-Gastaut syndrome and Dravet syndrome. And, a bipartisan proposal was introduced in Congress that would permit the Veterans Administration to study cannabis as a treatment for chronic pain and the symptoms of Post Traumatic Stress Disorder.
CBD vs. THC
So, after an 80-year prohibition, what has prompted all this attention? That can perhaps be attributed to a better understanding of cannabinoids, the compounds in the cannabis plant. Of the 100 or so cannabinoids the plant produces, THC has the psychoactive property that produces the high. It is the most familiar. Its compound counterpart, CBD is a non-psychoactive and has more therapeutic benefits. It is only in the past 20 years that science has identified that difference. Used together, CBD mitigates the high of THC, while enhancing cannabis therapeutic effects. That combination, in varying ratios of THC: CBD, is available in a wide range of commercial products.
Martin Lee, director of Project CBD and author of the acclaimed Smoke Signals: A Social History of Marijuana—Medical, Recreational and Scientific addressed the cannabis issue head on. “It’s no longer a question as to whether medicinal cannabis works,” says Lee. “It’s how to use it more effectively.”
 With cannabis listed as a Schedule I controlled substance, clinical research in the U.S. has been severely limited. Israel, and now Canada have taken the lead. “There have been discussions about changing cannabis to a Schedule II substance,” says Lee. “Though that would be significant and pave the way for long-suppressed research, it wouldn’t go far enough. Cannabis shouldn’t be considered a controlled substance at all. It should be regulated as a medicinal herb, not as a pharmaceutical or dangerous street drug.”
With cannabis listed as a Schedule I controlled substance, clinical research in the U.S. has been severely limited. Israel, and now Canada have taken the lead. “There have been discussions about changing cannabis to a Schedule II substance,” says Lee. “Though that would be significant and pave the way for long-suppressed research, it wouldn’t go far enough. Cannabis shouldn’t be considered a controlled substance at all. It should be regulated as a medicinal herb, not as a pharmaceutical or dangerous street drug.”
Cannabis can be used to effectively complement and interact with prescription medications. “Cannabinoid-opioid interaction shows great therapeutic potential,” says Lee. “THC enhances the painkilling effects of opiates, while CBD can reduce withdrawal and dependence. This could help solve the opioid addiction crisis, save lives and reduce the nation’s health-care costs.”
Medicinal products
CannaCraft is the largest producer of medicinal cannabis products in California. With 200 employees, the company operates out of a 36,000-square-foot facility in Santa Rosa. Bill Silver, formerly the dean of Sonoma State University’s School of Business and Economics, became chief executive officer in January 2018.
Kial Long is the company’s vice president of marketing. “After legalization of recreational cannabis in January, sales of our CBD-rich medicinal products doubled. Who would have imagined?” adds Long. “Perhaps pent up demand coupled with the availability of easy-to-use CBD applications could’ve been a part of what happened.” CannaCraft’s product range includes edibles, salves, vapes, tinctures and soft-gel capsules. Their Care-by-Design brand is the most popular among CBD users.
The CannaCraft production process starts in the extraction room where CBD-rich cannabis buds are placed in tall stainless steel cylinders. The room rumbles with the steady hum of environmentally friendly, high-pressured CO2 flowing through, extracting oil. The resultant residue is refined into a clear, golden liquid. The liquid is lab tested in accordance with standards set by California’s Bureau of Cannabis Control. Currently there are 20 extractors operating full time. “We’re planning to add 10 more in the next six months to meet the demand,” says Long.
Medicinal cannabis is widely used in California’s retirement communities. In 2015, Oakmont resident Tina Hoogs’ mother was diagnosed with colon cancer. Concerned because her mother was allergic to pain medications, Tina sought alternative relief. When Hoogs mentioned cannabis to the oncologist, he replied “great idea” and provided the medical card required by dispensaries at that time. Hoogs began slowly, with a drop of a tincture once a day. “And since my mother liked her sweets, I gave her a cannabis brownie at night to help her sleep.” Feeling rested throughout the day, Hoogs’ mother experienced no pain or anxiety. and maintained her appetite. Eventually, she lapsed into a coma; two days later she peacefully passed away. Seeing first-hand how medical cannabis helped her mother, Hoogs wanted to learn more and help others. She enrolled in a cannabis study program at Oaksterdam University; the school’s name is a derivative of Oakland and Amsterdam, the first two cities to legally support dispensaries. Since its inception 10 years ago, more than 35,000 students from 40 countries have graduated. Both on-line and on-campus courses are offered.
In 2017, Hoogs, along with Oakmont resident Jim Bryne, founded the Oakmont Cannabis Club. The Medical Marijuana Club established several years ago at Roosmoor, the active senior community in Walnut Creek, served as their model. Oakmont has 225 club members with ages ranging from 55 to 93. “Seems like membership increases at every meeting,” says Hoogs. A recent member joined after having a hip replacement. “She didn’t want to use opioids for pain,” Hoogs explains. “She was curious. She wanted to learn how cannabis might help.” Many members use sub-lingual drops or soft gel CBD to complement, or as a substitute for prescription drugs. Others apply salves for tennis elbow or for knees stiffened by arthritis. “CBD helps us stay active longer,” she says.
Past speakers at the monthly Oakmont Cannabis Club meetings have included doctors, representatives from dispensaries and product manufacturers. Marilyn Hutler, M.D., a recent speaker, is a retired Harvard-trained, board-certified anesthesiologist with 40 years of practice. In her own quest for pain relief, she discovered medical cannabis. And eight years ago Hutler opened a medical cannabis consultancy private practice. During that time, she has seen more than 15,000 patients.
Sonoma County is home to 20 cannabis dispensaries. Neither Marin nor Napa counties permit brick-and-mortar operations, though delivery services are allowed. At most dispensaries, products are kept behind the counter or secured in glass cases. For first time visitors, the scene can be intimidating. Not so at Solful the dispensary located in Sebastopol. The store has the welcoming, comfortable ambience of a Pottery Barn. Cannabis products are artfully displayed. Customers can spend time browsing and asking questions of the knowledgeable Health and Happiness Consultants.
Eli Melrod is the dispensary’s co-founder and CEO. He discovered cannabis at an early age. When he was growing up in San Francisco, his father was diagnosed with pancreatic cancer. He used cannabis for help with sleep, nausea and anxiety. Over time the cancer went into remission. “In 2015, I was trying to decide what I wanted to do with my life,” says Melrod. “The cannabis market was opening up in a big way. And seeing how cannabis helped my father, I wanted to help others.” He took a job at the Pure Analytics testing lab in Santa Rosa. There he received a crash course in all aspects of the cannabis business from growing, product screening, and distribution to applications. 
When California’s cannabis legislation passed in January 2018, Solfuls’ business quadrupled. “Our customers come from Marin, Petaluma, Napa, Santa Rosa and all over Sonoma County. Thirty percent are over age 60, another 55 percent are between ages 30 and 60, and the remaining 15 percent are Millennials,” says Melrod. New hires go through a training program based on a curriculum developed by a doctor familiar with cannabis medical benefits. The consultants also go on field trips spending time with product manufacturers and growers.
From wine to weed
One of those growers, and a valued Solful partner, is Glentucky Family Farm owned by Mike and Mary Benziger. Mike was former CEO of the Benziger Family Winery and a pioneer in the Sonoma Valley wine industry. In 2015, the family sold their 85-acre Glen Ellen winery to The Wine Group, the world’s second largest wine producer. That sale allowed Mike to turn his attention to other passions— biodynamic farming and growing cannabis.
Glentucky, located on eight acres on Sonoma Mountain, grows 30 different types of fruits and vegetables and has a garden with 50 cannabis plants. The farm (sans the cannabis) was certified by Demeter Biodynamic (BD) in 2001. The cannabis garden became certified in 2015. It’s the first cannabis-growing operation in the U.S. to receive the Demeter biodynamic certification. Rudolf Steiner conceived Biodynamic agriculture as a farming practice in Germany in 1924. Some describe it as a step above organic. The entire farm is certified, not just a single crop. Biodynamic farming regenerates and stimulates microbes in the soil. The greater the quantity and diversity of microbes, the denser the nutrition in the plants, and the food and medicinal benefits produced. In addition to fruits, vegetables and cannabis, the Benziger’s adapted a portion of Glentucky for use as a “pharmacy garden.” They’ve contracted with a well-known doctor in San Francisco to grow and sell medicinal plants for conversion into powders and capsules.
The couple’s interest in cannabis happened about seven years ago when Mike was diagnosed with two cancers, one of which had spread. “While undergoing the classic treatments, my anxiety increased. I couldn’t sleep well. And others with cancer also mentioned anxiety as being an issue,” Mike said. “So I turned to cannabis. Using trial and error I discovered a strain that reduced my anxiety.” That discovery became the impetus for Mary and Mike to start a garden and grow cannabis to help others. “At Glentucky we continue to experiment, searching for cannabis strains that grow best in Sonoma Valley’s climate and terroir. When I give talks and meet people, I’m surprised at all the interest, especially from the older generation,” Mike said. “Cannabis is one of those miracle substances, a gift that comes along once in a great while.”
 Courtney King, M.D., who started the Functional and Integrative family practice, Golden Road Medicine, located in Bennett Valley, spoke at a recent Solful dispensary event. Her topic—Cannabis and Women’s Health. “The plant that produces the cannabis buds is female,” King said with a smile. “So it’s only natural that cannabis could be good for women’s health.” She explained how cannabis can provide relief with PMS, hot flashes and cramps as well as issues related to menopause, like insomnia, mood swings and decreased sex drive. In her practice, King focuses on optimizing lab work, personalized food and diet plans, exercise and stress reduction for better health. “I mainly recommend cannabis and/or CBD for chronic pain, inflammation, anxiety and sleep.” King stressed that the much-touted benefits of cannabis have not been proven through medical research. Nonetheless, users are trying it, discovering the benefits and spreading the word.
Courtney King, M.D., who started the Functional and Integrative family practice, Golden Road Medicine, located in Bennett Valley, spoke at a recent Solful dispensary event. Her topic—Cannabis and Women’s Health. “The plant that produces the cannabis buds is female,” King said with a smile. “So it’s only natural that cannabis could be good for women’s health.” She explained how cannabis can provide relief with PMS, hot flashes and cramps as well as issues related to menopause, like insomnia, mood swings and decreased sex drive. In her practice, King focuses on optimizing lab work, personalized food and diet plans, exercise and stress reduction for better health. “I mainly recommend cannabis and/or CBD for chronic pain, inflammation, anxiety and sleep.” King stressed that the much-touted benefits of cannabis have not been proven through medical research. Nonetheless, users are trying it, discovering the benefits and spreading the word.
John Malanca and his late wife, Corinne, formed United Patients Group (UPG) in Marin in 2011. As with others who pursue medical cannabis careers, the company was set up following the experience of a family member. Corinne’s father, Stan Rutner, a retired Marin dentist, was diagnosed with Stage 4 lung cancer that metastasized to his brain. He was on oxygen full time and given two weeks to live. As Rutner was not in pain, there was no need for morphine.
“We read a study that showed 40 percent of cancer patients die from malnutrition caused by lack of  appetite/wasting syndrome. We didn’t want that to happen to Stan,” says Malanca. “Corinne and I had no experience with cannabis. It wasn’t a part of our lifestyle. But with no other option, and after getting the okay from the Kaiser oncologist, we gave Stan a coconut oil capsule infused with cannabis—about 3 mg each before breakfast each day in hopes of increasing his appetite. Within 24 hours he was eating. We thought, perfect, he will pass peacefully. By day eight, not only was he eating, his strength came back, his mood and his will to live was there. He started getting out of bed and walking-shuffling through the house.
appetite/wasting syndrome. We didn’t want that to happen to Stan,” says Malanca. “Corinne and I had no experience with cannabis. It wasn’t a part of our lifestyle. But with no other option, and after getting the okay from the Kaiser oncologist, we gave Stan a coconut oil capsule infused with cannabis—about 3 mg each before breakfast each day in hopes of increasing his appetite. Within 24 hours he was eating. We thought, perfect, he will pass peacefully. By day eight, not only was he eating, his strength came back, his mood and his will to live was there. He started getting out of bed and walking-shuffling through the house.
“Something is working,” Rutner remarked one day. At six months, we incorporated a drop of cannabis oil (a 4:1 ratio of THC:CBD). At nine months, Stan went behind our backs to get scanned, the results—no evidence of recurrent disease!” Malanca follows with a caveat. “I don’t want Stan’s story to infer that cannabis cures cancer. No one knows why one person goes into remission, and someone else doesn’t. What cannabis did was to maintain Stan’s appetite. And that kept his strength to fight the battle.”
Malanca is host of a seven-part documentary titled, The Sacred Plant: Healing Secrets Exposed. The series, available for viewing at www.TheSacredPlant.com, chronicles the experiences of medical professionals, scientists, government officials and patients from around the world. UPG also does patient consultations through its network of cannabis-trained professionals, and conducts educational conferences on college and university campuses as well as medical and government institutions.
(For more up-to-date information, visit the UPG website at www.unitedpatientsgroup.com.)
Once known by the slang terms “weed” or “pot,” the herb has achieved respectability and is now more commonly called cannabis, the botanical name of the plant it comes from. And it’s no longer used just for recreational purposes. It’s more widely used for its medicinal benefits. Perhaps the Haight-Asbury hippies were on to something, though too stoned to detect the therapeutic CBD that lurked beneath the haze.
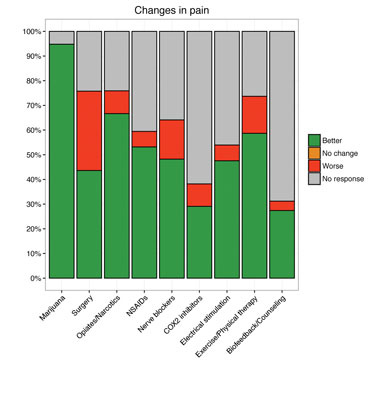
changes in pain
In a 2016 Care by Design and Project CBD report, 800 people were surveyed on the use of cannabis and other therapies to treat age-related pain. Most survey respondents were between 50 and 70 years old. The vast majority—83 percent—reported suffering from chronic pain; half reported suffering from acute pain; 42 percent reported suffering from both. On average, respondents had tried four different treatment methods for their pain. Twenty-five percent of respondents reported having tried six or more.
what is project cbd?
 Project CBD is a California-based nonprofit that provides and publicizes up-to-date research on the medical uses of cannabidoil, or CBD. Their website, www.projectcbd.org, is a reliable educational source of information for physicians, patients and the general public. Project CBD, recognizing that many health-care professionals have little or no experience with cannabis therapeutics, assembled a beginner’s guide to address CBD user’s questions.
Project CBD is a California-based nonprofit that provides and publicizes up-to-date research on the medical uses of cannabidoil, or CBD. Their website, www.projectcbd.org, is a reliable educational source of information for physicians, patients and the general public. Project CBD, recognizing that many health-care professionals have little or no experience with cannabis therapeutics, assembled a beginner’s guide to address CBD user’s questions.
is cannabis addictive?
Cannabis has been touted for its medicinal benefits for years, but if you’re a user the question remains: Is cannabis addictive? Some say that cannabis can be addictive, though there is insufficient evidence to support that claim one way or the other.
Leslie L. Iverson professor of pharmacology at the University of Cambridge and author of “The Science of Marijuana” states that 9 percent of marijuana users become addicted— much less than for other substances. Estimates are that 32 percent of tobacco smokers struggle with addiction, 23 percent for heroin users, 17 percent for cocaine and 15 percent for alcohol. Cocaine and heroin are the most physically harmfully; nicotine is the most addictive. It’s more difficult to quit smoking cigarettes than to stop smoking pot.
So why is it that some people become substance addicts and others don’t? A definitive answer to that question has long been debated, and not just for marijuana. The Mayo Clinic states that marijuana addiction occurs in 10 percent of those who begin smoking pot prior to age 25. Baby Boomers and others would question that. And there’s research suggesting that 90 percent with an addiction to marijuana have another addiction such as alcoholism, or a mental illness such as an anti-social personality disorder.
On another note, cannabis is being used to reduce or eliminate reliance on other more harmful substances such as alcohol, cocaine, and heroin. With cannabis illegal at the federal level, there are few reliable studies available. The benefits and risks of cannabis should be considered as a part of a national discourse. More comprehensive, unbiased research is needed. In the meantime consumers, particularly the older generation, are becoming educated on the subject. They’re weighing the risks, exploring the benefits and using cannabis for a range of ailments.
the other side
The discussion over cannabis as medicine is still hotly debated. On the one hand, there’s the group who believes it should be accessible to patients whose doctors recommend cannabis to improve medical conditions. On the other hand, there are those who are strongly opposed to medical marijuana.
According to the World Health Organization (WHO), cannabis is the most widely cultivated, trafficked and abused illicit drug. Half of all drug seizures worldwide are cannabis seizures. What’s more, the geographical spread of those seizures is also global, covering nearly every country of the world. About 147 million people, 2.5 percent of the world’s population consume cannabis (annual prevalence), compared to 0.2 percent consuming opiates. In the present decade, cannabis abuse has risen faster than cocaine and opiate abuse. Since the 1960s, the most rapid growth in cannabis abuse is in developed countries such as North America, Western Europe and Australia.
Acute health effects
The acute effects of cannabis use have been recognized for years. Recent studies confirmed and extended the following earlier findings that cannabis:
Impairs cognitive development (capabilities of learning), including associative processes; free recall of previously learned items is often impaired when cannabi is used both during learning and recall periods.
Impairs psychomotor performance in a wide variety of tasks such as motor coordination, divided attention and operative tasks; human performance on complex machinery can be impaired for as long as 24 hours after smoking as little as 20 mg of THC in cannabis. Additionally, there’s an increased risk of motor vehicle accidents among persons who drive when intoxicated by cannabis.
Chronic health effects
There are a number of risks to chronic use of cannabis, according to WHO. Some of those risks include:
Development of a cannabis dependence syndrome, which is characterized by a loss of control over cannabis use.
Injury of the trachea and major bronchi caused by long-term cannabis smoking.
A higher prevalence of symptoms of chronic bronchitis and a higher incidence of acute bronchitis among those who smoke cannabis, compared to those who don’t.
Exacerbated schizophrenia in affected individuals.
For more information, visit www.who.





