
Artificial intelligence is all around. Ask Siri a question on an iPhone or give Google’s Alexa an instruction, and AI comes into play as an electronic personal assistant to meet one’s needs.
ChatGPT makes jobs like writing reports easier, and AI can analyze large amounts of data quickly and efficiently to recognize patterns and reach conclusions. In health care, it’s able to evaluate images and identify areas of concern, often at the crucial early stages of disease, giving physicians new tools to help save lives and prevent the life-altering consequences of undetected conditions. In addition, AI is making tedious tasks—such as transcribing medical records—a thing of the past by converting audio to text rapidly, freeing employees to spend their time on more meaningful work.
AI is specialized software that allows computers to replicate human intelligence by using algorithms—the commands a computer follows—to complete tasks. It has access to large volumes of data sets and, when programmed with the correct questions, it can use the data to focus on solving a specific problem. As it processes masses of information, it also learns from it to do its assigned tasks better, so its ability improves over time. It’s able to analyze large quantities of data much faster than people and is typically more accurate, partly because machines don’t get tired or have interruptions to the workflow the way multi-tasking humans do. The goal, though, isn’t to replace people. Rather, in healthcare, AI is a tool that assists medical professionals by providing valuable information quickly so they can use it to enhance their decision-making—resulting in better outcomes and benefiting patients.
Evolution
Although AI has only become mainstream in the public consciousness in recent years, as an area of computer science, it’s far from new. The term artificial intelligence was coined in 1956 and the Department of Defense began exploring possible uses in the 1960s. The Defense Advanced Research Project Agency took advantage of AI to do street-mapping projects in the 1970s, and the first application in healthcare came in the same decade with the development of an AI program that identified blood infections. In 1979, the American Association for the Advancement of Artificial Intelligence (haaai.org) came into being, and AI continued to advance in the 1980s and ‘90s with research on methods to collect and process data faster and assist in making some medical procedures more precise. For instance, robotic surgery such as the DaVinci system, which augments a surgical team’s capabilities, was in use in operating rooms in Europe in 1999 and received approval from the U.S. Food and Drug Administration in 2000. Progress was slow but steady until 2011, and then AI began to get the public’s attention when breakthroughs in deep learning—also known as strong AI—modeled on the human brain made it possible for computers to perform tasks using images, text and sound. Its use accelerated, and several areas of healthcare, including primary care, radiology, screening, the diagnosis of disease and telemedicine, now use it as an integral part of their practices.
When time counts
Patients having strokes lose more than a million brain cells a minute, so the faster they get treatment the better. AI is a gamechanger in such cases, because in providing images quickly, it allows a physician to put a treatment plan into action sooner than is possible with traditional methods. Stroke specialists in Sutter Health’s network are using an AI-based platform that automatically processes CT scans to identify large blood-vessel clots and deliver clear images that are easy to interpret. “Hospital stroke teams and emergency department personnel receive these results in three minutes or less,” says Laura Wilt, a senior vice president and Sutter’s chief digital officer. “This rapid response enables doctors to diagnose the stroke type and plan treatment faster and more accurately,” she explains, giving victims a better chance of recovery.
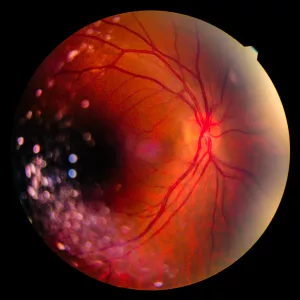
In imaging, AI can find subtle abnormalities that are difficult for the human eye to see. The National Institutes of Health, a federal agency noted for its medical research, reports that physicians are using retinal scans to identify diabetic retinopathy, a complication of a type of diabetes that causes lesions on the retina and can lead to blindness if not caught early. Ophthalmologists can diagnose the condition manually, but it’s a lengthy, costly process with the risk of misdiagnosis, and AI’s deep learning has produced more accurate results. In addition, the NIH reports that AI can analyze routine eye scans to spot changes in the retina’s tiny blood vessels that are a sign of vascular disease and identify patients at risk for heart attacks.

AI also shows promise in helping diagnose cancer early, and the NIH reports that studies using AI and Machine Learning—a subset of AI—have been highly accurate in finding several types of the disease, including breast, brain, lung, liver and prostate cancer. The NIH encourages developing the technology further, and in 2020 Sutter Health partnered with Ferrum Health in San Francisco to study ways to find tumors at earlier stages.
MarinHealth Medical Center is using AI solutions in key areas that include diagnosis assistance, imaging enhancement and patient monitoring, such as rapid response of warning systems in the ICU. Provider documentation and virtual scribes, predictive analytics for population health and length-of-stay monitoring and alerting, as well as clinical-decision support, are additional areas where AI is delivering benefits.
MarinHealth is also using new technologies in cardiac care, which include AI image-guided technology for detecting Abdominal Aortic Aneurysms (AAA) and a cardiac MRI program that increases scanning throughput (the amount of data that goes through a computer) for myocardial function with quick ejection fraction, stroke volume and mass calculations. “This means physicians will have access to enhanced images and more accurate data regarding a patient’s heart and its function to make better, more informed decisions regarding patient care,” says a statement from MarinHealth.
Also in cardiology, the Mayo Clinic reports using AI techniques in a screening tool that identifies left ventricular dysfunction and in an Apple Watch to detect a weak heart pump. In addition, its studies show that AI-guided electrocardiograms can detect faulty heart rhythms before a patient becomes symptomatic.
Lightening the workload
AI’s streamlining of administrative tasks provides benefits for both medical personnel and patients. It can estimate the amount of time a particular surgery will take, for instance, allowing improved operating-room schedules and shorter wait times. When physicians record their observations and appointment notes, AI can use natural language processing to transcribe them and post the records on online portals, giving both doctors and patients access to medical records. And because machines can work 24 hours a day, the information is available quickly.
“Administrative tasks consume a significant portion of clinicians’ workdays,” says Wilt, and she explains that Sutter is using AI to improve in-basket workflows and complete the documentation requirements that regulations and insurers require. Sutter is also working on a pilot project with Epic, a Wisconsin-based company that specializes in electronic health records and produces software for hospitals. “More than 60 Sutter-affiliated physicians are testing generative AI methods to respond to patient messages,” she reports, explaining that the Epic software uses AI to analyze the content of messages from patients and draft responses based on their charts and history. Doctors then review and send the final response. She adds that Sutter is experimenting with generative AI technology, such as ChatGPT, to automate clinical documentation as well. “This exciting initiative is a practical step toward transforming how physicians work and interact with patients, focusing on automating administrative tasks during patient visits,” she says.
With technology a part of everyday life, Wilt finds that patients expect to it to have a role in healthcare and the way they access it as well. “Sutter is proactively responding to these expectations with our digital strategy and evolving technologies, including AI, with the goal to provide a seamless, high-quality patient experience,” she reports. “Our approach revolves around elevating the entire healthcare experience for patients and our care teams. We see endless opportunities to deliver an even more personal, connected and convenient experience.”

UCSF MarinHealth announced in August 2022 that it would begin using APeX, a version of Epic EHR created specifically for its system. It gives patients access to their medical records through MyChart, an online portal that keeps all their medical information in one place. They can see tests results, schedule appointments, send messages and request prescription renewals simply by logging onto the portal on their personal devices at their own convenience. Clinicians also have access and can see detailed information, such as patient records, notes from other doctors, current prescriptions and upcoming appointments with specialists. AI thus provides a big picture that helps them to make better diagnoses and decisions about treatment.
Looking ahead
Among its applications, Kaiser Permanente is using AI natural language processing to analyze email messages from patients to identify their areas of concern so that the best person responds. It is also using predictive analysis to develop algorithms that can evaluate COVID-19 patients and identify those at risk of developing more severe symptoms. Creating and evaluating algorithms using AI and ML are a focus of Kaiser’s Division of Research, and the stated goals of its Augmented Intelligence in Medicine Initiative, which is located in Northern California, are “to advance research methods, identify best practices and build capacity for effectively implementing and rigorously evaluating the use of AI/ML algorithms for diagnostic decision-making in real-world settings.”
In December 2023, AIM-HI announced that it had awarded grants of up to $750,000 to allow five healthcare organizations across the country to carry out research projects using AI and ML. One project, at Parkland Health in Dallas, involves an AI/ML model for pediatric asthma care in safety net health settings, and the use of AI in diabetic retinopathy screening is the focus of another at San Ysidro Health in San Diego. The funding is for three years, and AIM-HI’s advisory committee will provide support by sharing best practices and lessons learned and advancing the use of AI and ML in healthcare.

Looking farther into the future, the World Economic Forum’s annual meeting in Switzerland in 2020 predicted three major ways that AI will change healthcare by 2030. First, AI predictive care will identify factors such as inherited medical conditions, diet, the environment, income and stable housing, which can impact health, allowing physicians to recommend measures that patients can take to help prevent a disease from developing. Second, digital networks will connect healthcare centers, including hospitals, same-day surgery centers, clinics and even patients’ homes, so patients can get care at the most appropriate location, and healthcare personnel can go to the spot where they are needed the most. Third, good experiences aid recovery and create a better workplace, and AI will provide better experiences for both patients and staff, as it reduces wait times, improves workflows and takes on more administrative tasks to relieve the burden on employees.
“By learning from every patient, every diagnosis and every procedure, AI creates experiences that adapt to the professional and the patient. This not only improves health outcomes, but also reduces clinician shortages and burnout, while enabling the system to be financially sustainable,” the report concludes.
Innovation and initiatives that explore new uses make the future of AI in healthcare look bright—yet it still has challenges. A human programmer must set up the system and ask the right questions without bias to create a well-constructed algorithm that will produce the desired results—so even highly sophisticated software has the risk of error. In addition, audio recordings need to be high-quality and clear, with a speaker who articulates well, for computer transcription to be accurate, although doctors usually have an opportunity to review reports and make corrections. And in identifying problem areas on scans, the minute detail AI analysis provides can produce more information than a physician needs. Worries about privacy and security are also an issue.
MarinHealth reports that it takes a rigorous and principled approach to evaluating the security, effectiveness, ethics and potential outcomes of any new AI adoption and development. To do so, it has gathered a cross-functional team of experts to ensure that any initiative is safe and feasible within its technology framework and that the expected workflow will benefit clinicians in helping them make better decisions in caring for their patients.
Oversight
The FDA is responsible for the oversight of software in healthcare and has approved many of the AI products currently in use, although not all. The 21st Century Cares Act, which Congress enacted in 2016 to provide substantial funding for research to the NIH, exempts many AI tools from FDA regulation if healthcare providers don’t rely on them to make diagnoses or decisions on treatment. In 2022, however, the FDA announced that it would categorize some types of tools—such as smartwatch software that uses data from electrocardiograms to detect arrhythmias—as medical devices, so greater scrutiny is likely as the use of AI grows. In October 2023, the FDA announced that it had reviewed and approved 171 AI and ML-enabled medical devices, including the irregular rhythm notification feature on Apple’s watch. The FDA released the list as a service to the public and reports that its review focused on the devices’ overall safety and effectiveness.
“Digital health technologies are playing an increasingly significant role in many facets of our health and daily lives, and AI/ML is powering important advancements in this field. Ensuring that these innovative devices are safe and effective and that they can reach their full potential to help people is central to the FDA’s public health mission,” the announcement says.
Despite the growing pains, AI has the potential to provide groundbreaking innovations that do a great deal of good and ensure better outcomes—much as X-rays, mammograms and vaccines did when they were first introduced. It holds the promise of more to come, but AI is already making a difference, and as time goes on, functions that once seemed to be in the realm of science fiction could very well become reality.



