For a tiny organism, SARS-CoV-2 has had an incredible impact on the world. It emerged as a novel coronavirus in Wuhan, China, in December 2019, and at the outset, even before it had spread abroad, the global medical community recognized it might be the beginning of a new pandemic. Such a scenario was inevitable. Global outbreaks, such as the Black Plague, have occurred throughout history. And because the last major pandemic was more than a century ago—the Spanish Flu of 1918, took the lives of roughly 500 million people worldwide—we were due for one. The problem, though, is that no one knows when a pandemic will strike, where it will start or what form it might take, so it’s all but impossible to stop a virus at its source.
Infectious disease specialists are knowledgeable about the precautionary measures necessary to help limit the spread of a virus once it emerges, but finding out how a new one behaves is the key to finding ways to control it. That process takes time, and medical professionals spent much of 2020 performing research to determine the best methods to treat the disease effectively and develop a vaccine to halt the virus’ spread. Now, they know substantially more about SARS-CoV-2 and COVID-19, the disease it causes, than they did in January, when the Centers for Disease Control and Prevention (CDC) confirmed the first case in the United States.
Learning curve
Severe Acute Respiratory Syndrome Coronavirus—SARS-CoV—was the first coronavirus of its type, and it caused an epidemic in 2002-2003 that led to 800 deaths. SARS-Cov-2 is the second, and as a novel coronavirus, it has some similarities to the first as well as its own unique qualities. Like the earlier coronavirus, it jumped from animals, possibly pangolins, to humans and is spread through the air. Its effect, however, is less predictable. Infection results in a wide range of symptoms, so while some individuals don’t become sick at all, it’s lethal for others, especially older adults.
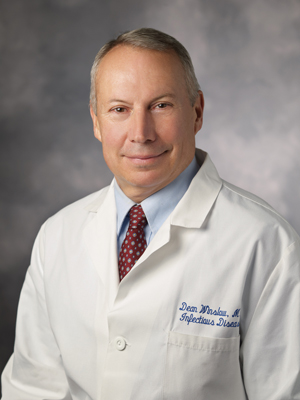
Dean Winslow, M.D., professor of medicine, division of infectious diseases and geographic medicine at Stanford University School of Medicine, explains that COVID-19 is a respiratory infection resulting from the transmission of small-particle, virus-laden aerosols and large-particle droplets. The new coronavirus is extremely easy to transmit because people who are infected expel aerosols and particles that are shedding virus into the air when they speak, cough or sneeze, even if they don’t have symptoms.
 Indoors, the virus stays suspended in the air for three to four hours, creating an especially high-risk environment. He gives the example of a choir practice in Skagit County, Wash., in March, which 61 people attended. It lasted two-and-a-half hours, and one person with cold-like symptoms infected 53 others with SARS-CoV-2. “Some were as many as 40 feet away from the index patient,” says Winslow, but others were only a few inches apart. Singers expel more aerosols and droplets than someone who’s speaking, and he believes the spread was the result of members having prolonged exposure to the virus indoors.
Indoors, the virus stays suspended in the air for three to four hours, creating an especially high-risk environment. He gives the example of a choir practice in Skagit County, Wash., in March, which 61 people attended. It lasted two-and-a-half hours, and one person with cold-like symptoms infected 53 others with SARS-CoV-2. “Some were as many as 40 feet away from the index patient,” says Winslow, but others were only a few inches apart. Singers expel more aerosols and droplets than someone who’s speaking, and he believes the spread was the result of members having prolonged exposure to the virus indoors.
Infection occurs when a host inhales the virus, and it binds to a human cell and replicates. As it grows and gains strength, the virus attacks the lungs, but it can affect the heart and other tissues, too. “It appears to activate the clotting system,” says Winslow. The resulting blood clots can harm the organs, leading to heart attacks, strokes or kidney damage. So far, it’s unknown whether the clots form as a direct result of the coronavirus or if they are an immune system response.
Inflammation is the mechanism that the immune system uses to protect the body from viruses and fight off disease. An excess is counterproductive, however, and a substantial amount of inflammation is associated with SARS-CoV-2. Eric Verdin, M.D., president and CEO of the Buck Institute for Research on Aging, explains in his blog that the body has two immune systems.
The first is the innate immune system, and one of its major features is inflammation, which Verdin describes as “a cellular response that alerts the rest of the system that there’s a problem.” He explains that the innate immune system changes as people age and also in those infected with SARS-CoV-2, which can cause an increase in its responses, resulting in chronic inflammation and limits its ability to fight infection. “A key factor that determines a poor prognosis during COVID-19 is a hyperactive innate immune system,” he says. The adaptive immune system is the second line of defense, and as one ages, a decrease in its responses means the cells that create and remember pathogens die off without dividing, making them less able to repel foreign pathogens. Thus, both immune systems are diminished, making older adults more vulnerable to becoming critically ill if they develop COVID-19.
Seniors at risk
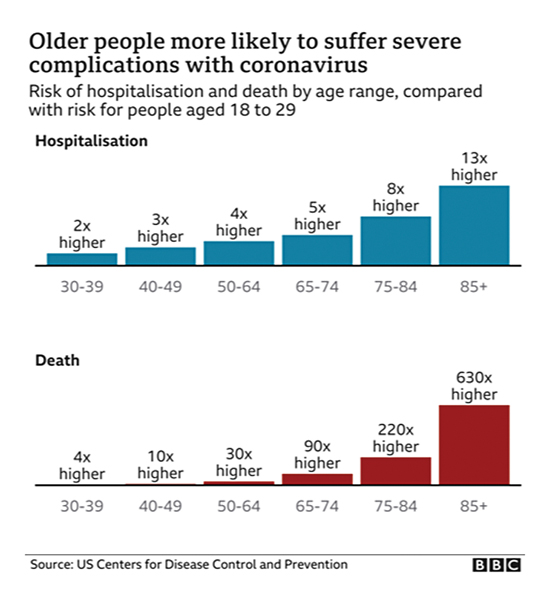
The elderly were suspected to be the most at risk at the beginning of the pandemic, but as time went on, the age of infection dropped, and the number of cases increased in younger age groups. The CDC reports that persons age 20 to 29 had the highest number of cases in July and August, accounting for more than 20 percent of all cases nationally. The number of older adults becoming infected was significantly lower, but other underlying chronic medical conditions increase their risk and they tend to get more seriously ill with a higher mortality rate. People age 65 to 74 are 90 times more likely to be hospitalized and die than adults aged 18 to 29, and that increases to 630 times for seniors older than 85. The CDC reports that adults age 65 and older account for eight out of 10 deaths and urges them to be diligent in taking the measures necessary to avoid becoming sick.
Outbreaks in skilled nursing and assisted-living facilities in the North Bay were responsible for many of the early cases of COVID-19. Contact tracing showed that the residents who were infected usually contracted the virus from the same individual, while employees were exposed to various outside sources. Now, many nursing homes have their own testing equipment to monitor both residents and staff more closely. Lisa Santora, M.D., deputy chief of public health, Marin County Health and Human Services, explains that while most people under the age of 50 develop infection and increase their viral load within seven days, the response is more blunted in older adults. As a result, the challenge is determining the frequency of testing that yields the best results.
The federal government sent some early antigen tests to skilled nursing facilities, Santora reports, but they have a high false-negative rate when used for screening, so it’s possible for a person to be infected but have a negative test result. Antigen tests detect certain proteins in the virus and are faster and less expensive than PCR (polymerase chain reaction) tests, which use a lab technique to detect the genetic material of the virus. That makes antigen tests practical for large numbers of people, but PCR tests are more accurate. Skilled nursing facilities have increased testing, however, and if they have an active outbreak, Marin Health and Human Services partners with them to test residents twice a week.
Sundari Mase, M.D., health officer for Sonoma County, points out that the problem in skilled nursing facilities and residential care facilities for the elderly (RCFEs) is that employees who don’t display symptoms might be infected but not know it and unwittingly pass on the virus to residents. As a result, both types of facilities are doing surveillance testing regularly. During public comments on Oct. 30, she reported that 50 percent of the staff is tested every two weeks at skilled nursing facilities, and 25 percent of the employees get tests each week at RCFEs. “They’re testing 100 percent of their staff monthly, basically,” she says.
“It’s terrible and heartbreaking that we have deaths in these facilities,” Mase adds. This fall, Sonoma County received 135,000 antigen tests for diagnostic purposes from the federal government, some of which went to skilled nursing facilities. “It’s to be used in symptomatic individuals within a week of symptom onset. It has to be an individual who is already sick,” she says. “It offers another alternative for a testing platform.” She also advises people who think they might have been exposed to a carrier to get tested, but not right away. It can take from two to 14 days for symptoms to emerge, so the best time to get tested is around day 12, Mase stated publicly on Nov. 4. Meanwhile, they should quarantine and take the measures necessary to stop the chain of infection, especially as the weather gets colder. If they’re unable to keep away from other people while waiting for a test result, the county offers options. Among them, the county has contracted with local hotels to house people during quarantine. “We’d like to have more people taking advantage of those,” Mase says.
The best strategy is prevention, and Santora advises older residents to be vigilant. “As things reopen, [seniors] need to thoughtfully determine which activities they increase,” she says. Forgoing social activities such as family gatherings might mean missing treasured traditions. “I would recommend not having the usual gatherings for the holidays.” One of the big risks is second-generation transmission, she explains, which occurs when seniors are exposed to younger people who could unknowingly infect them. She acknowledges that pandemic fatigue is an issue, causing people to struggle physically and mentally, as they miss spending time with family and friends and giving them hugs. “This disease is preventing us from doing that.”
However, Santora cautions that this is exactly the time to double down and avoid being careless. Otherwise, a second wave of infection is likely. No one anticipated a pandemic of this scale, she points out, and we have to make sacrifices. “Covid is a bit of a trickster,” she says. “We have to stay on our toes and keep on guard.” If people absolutely must get together during the holiday season, she advises wearing heavy coats, staying outside and using umbrellas if need be while remaining socially distanced with masks.
Vaccines
Beating SAR-CoV-2 requires creating herd immunity, and the only reliable method for achieving it is with a vaccine. The number of people who have been infected so far is well below the threshold required for creating herd immunity, and Winslow estimates that 90 percent of the population is still susceptible to the virus. He believes people who have recovered from COVID-19 probably have some immunity, but no one knows how much or how long it might last. A handful of people report being reinfected, suggesting that it could be short-term. Scientists don’t know enough yet to provide a definitive answer.
The nature of a coronavirus makes it unlikely that any immunity would be permanent; therefore, the goal is to develop a safe, effective vaccine. A recent report from researchers at the Imperial College of London included a model showing that without any preventive measures, the novel coronavirus would have infected 7 billion people and killed 40 million worldwide in 2020. “We don’t want to get to herd immunity through mass infection,” says Winslow. “We’re pinning our hopes on a vaccine.”
The director of the CDC, virologist Robert Redfield, M.D., participated in the Buck Institute’s COVID Webinar Series in July, and he emphasized the importance of vaccines. “It’s the most powerful tool we have, one of the greatest gifts modern medicine has given mankind,” he says. He reports that several different types of vaccines are being developed and tested using various platforms, since some work better than others for different populations. He expects at least five vaccines to be available and explains that while a vaccine might not prevent people from being infected, it would lessen the effects and prevent people from becoming severely ill and dying. “If it’s like a bad cold for a week, it would be satisfactory,” he says.
The challenge is convincing enough people to be immunized, and that requires a shift in the discussion about vaccines in general. Fewer people get the measles vaccine than those who don’t, for instance. “We need to get the American public to embrace the flu vaccine,” says Redfield, who is a senior himself and gets vaccinated yearly. He reports that the current vaccination rate is low, and if people with the flu have to be hospitalized, the capacity for COVID-19 patients would be reduced, and the health system could be overwhelmed. “If we get vaccinated, we’re less likely to have to go to the hospital.” Several vaccines are in trial phases, and he stressed that the process will not skip any scientific integrities or safety measures. “None of us are going to compromise safety,” he says. “What we are willing to compromise is money.”
Winslow explains that the vaccines under development for SARS-CoV-2 use one of four platforms. “My sense is that all four types will be reasonably safe.” He points out that they might differ in efficacy, but it’s important to wait for the completion of Phase 3 trials to learn more. He observes that the Food and Drug Administration (FDA) has been under political pressure to give early approval, but believes it will not allow any vaccines to be released if they are not safe.
Anthony Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases, shared that belief when he took part in a Commonwealth Club of California webinar in August. “There’s a difference between having a vaccine and having a vaccine that’s safe and effective,” he said, explaining that vaccines have to be tested properly to ensure safety and efficacy, and it would be irresponsible to distribute one before it had gone through that process.
Neither Fauci nor Redfield predicted when a vaccine might be available, but on Nov. 9, Pfizer Inc. and its partner BioNTech SE announced that initial Phase 3 trials on an mRNA-based vaccine, which targets the proteins in the virus’ spikes, showed it to be 90 percent effective. Trials are continuing, but, meanwhile, they anticipated asking the FDA for emergency use authorization (EUA) in late November. The FDA issues such an authorization when no adequate alternatives are available and the therapy shows promise, with benefits that appear to outweigh the potential risks.

In keeping with the national trend, the number of residents in Marin County getting immunized against influenza is low. “On our best year, only 50 percent of residents get the flu shot,” says Santora. She strongly recommends it and reveals that her target this flu season is 90 percent. It’s an ambitious goal, but it’s a strategy that could have tremendous impact. “The one thing we do know is that’s effective and will prevent a surge.” It would also help avoid a twindemic, with cases of the flu and COVID-19 at the same time. She suspects that it might take time for some people to accept a COVID-19 vaccine, however, because they will be hesitant to try something new. “Marin County public health will be making recommendations on vaccines only when we are confident that the benefits outweigh any risks associated with the vaccine,” she says. Santora explains that local public health officials rely on information from two federal bodies, the FDA and the Advisory Committee on Immunization Practices, a CDC committee, and they will review the science involved in clinical trials. “I would assure the public that our recommendation will be based on the best science and research,” she says.
Mase also urges people to get the flu vaccine. “It’s very important in this time of Covid that everyone gets vaccinated. You’ll be protecting yourself as well as the ones you love and the community,” she says. In addition, it will make diagnosis easier for people who get sick. “You don’t want to have a question about whether it’s Covid or the flu or maybe both.”
Remedies
As people continue to get sick, finding effective treatments is crucial. Remdesivir, a therapy that showed early promise, has proven to be successful. “If you start earlier, it probably works better,” says Winslow, He also reports that another important finding is the beneficial effect of corticosteroids, such as Dexamethasone, which help with moderate to severe symptoms. Corticosteroids have anti-inflammatory and immunosuppressant effects and are used for patients who are on oxygen or ventilators. In addition, on Nov. 9, the FDA it issued an EUA for Bamlanivimab, a treatment for COVID-19 in adults and children over 12 with mild to moderate infection. It’s useful for patients 65 and older and for those with chronic medical conditions, and it’s not for people who are at risk of developing more severe symptoms and being hospitalized. It uses a protein created in a laboratory to replicate the immune system’s response to infection and prevents the novel coronavirus’ spikes to attaching to human cells.
“All of us have become better at managing these patients in a general sense,” says Winslow, who notes that the mortality rate seems to be lower that it was initially. Findings by researchers at New York University Grossman School of Medicine confirm Winslow’s observation on improvements in case management. Their study revealed that the death rate for patients hospitalized with coronavirus-related illnesses had dropped significantly, from 25.6 percent in March to 7.6 percent in August. They determined that the improvement was partly the result of younger, more resilient people becoming infected, but they also discovered that as medical personnel gained experience and learned more, they became better at managing the disease.
COVID-19 continues to be a threat, however, and until a vaccine is available and its widespread use begins to have an effect, the best remedy for avoiding illness is to follow the commonsense rules: wear a mask, maintain social distance and wash your hands. “Wearing facemasks is going to be critically important until we get a vaccine,” says Winslow. They reduce the transmission of the virus from an infected person to another, he explains, and provide some protection for the wearer as well because they reduce the number of virus-laden particles an individual inhales. “Face masks are very important from an altruistic viewpoint and are also a benefit to the wearer.” Winslow also believes that to contain the virus, being slow and deliberate in deciding to reopen businesses and schools and allowing large indoor events is the wisest course.
Should one become ill, contact tracing is extremely important for controlling the spread of SARS-CoV-2. Nonetheless, Santora finds that many people aren’t reporting their close contacts, and she suspects they fear repercussions if others have to quarantine. “The strongest tool is isolation and quarantine,” she says. In addition, some people still underestimate the severity of the disease and don’t believe protective measures are necessary, which also harms the community’s recovery from the pandemic.
“This will end”
Fauci describes the path to understanding SARS CoV-2 and COVID-19 and finding ways to deal with them as a learning process. “As the weeks go by, we learn more and more, and as you get more experience, the knowledge changes,” he says, explaining that researchers start seeing things they didn’t early on. In past pandemics, it has taken about two years to contain a virus, and Winslow, Redfield, Santora and Fauci all expect a similar timeframe for SARS-CoV-2. “This will end,” says Fauci, but until it does, he recommends that members of the community stay engaged and be part of the dialogue so they will be informed and understand why each individual has a role to play.
“Don’t despair,” he says. “We will get through this.”